Testosterone is a fundamental hormone in male physiology, shaping numerous biological functions essential for health, vitality, and reproduction. As the primary male sex hormone, it plays a crucial role in muscle development, bone density, red blood cell production, libido, and overall well-being. However, many individuals are unaware of the intricate processes behind testosterone synthesis and the key structures responsible for its production. Understanding where testosterone is produced in males, the types of hormones involved, and how the body regulates this essential androgen provides deeper insight into male health and longevity.
You may also like: How to Get Your Testosterone Levels Checked: Best At-Home and Lab Testing Options
The Primary Site of Testosterone Production: The Testes
The testes are the principal structures in which testosterone is produced in males. Located in the scrotum, the testes contain specialized cells responsible for synthesizing and secreting testosterone into the bloodstream. These glands are vital not only for testosterone production but also for sperm generation, collectively influencing male reproductive function. Within the testes, Leydig cells play a crucial role in producing testosterone in response to hormonal signaling from the brain. Without proper testicular function, testosterone levels may decline, leading to various health issues, including reduced libido, muscle loss, and fatigue.
Leydig cells respond primarily to luteinizing hormone (LH), which is secreted by the pituitary gland. This interaction is a vital part of the hypothalamic-pituitary-gonadal (HPG) axis, a complex feedback system regulating testosterone levels in the body. When testosterone levels dip below an optimal threshold, the hypothalamus signals the pituitary gland to release more LH, stimulating the Leydig cells to produce additional testosterone. This dynamic regulatory system ensures that testosterone levels remain within a functional range to support male health.

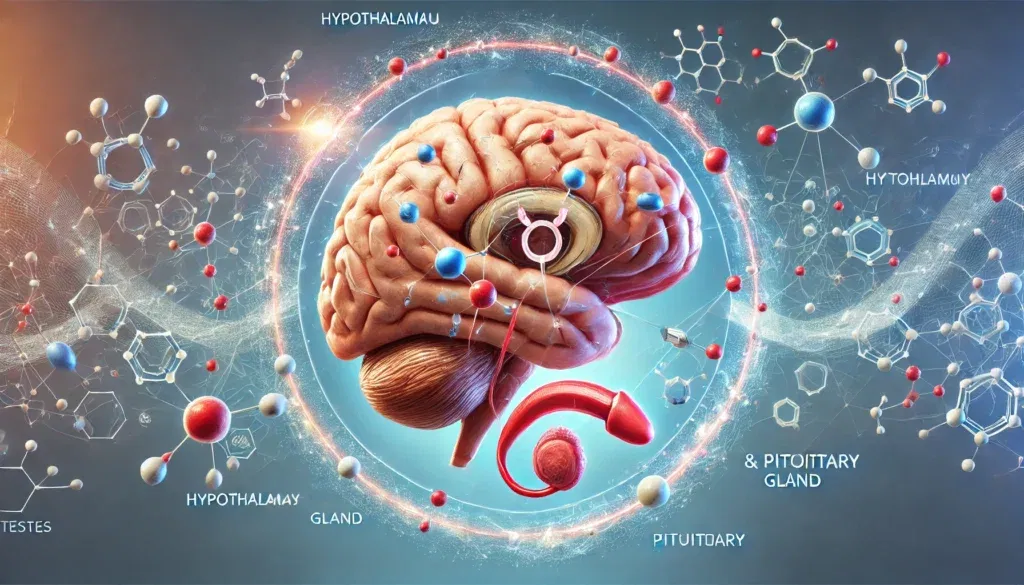
The Role of the Hypothalamus and Pituitary Gland
While the testes are the primary site where testosterone is made, they do not function in isolation. The hypothalamus and pituitary gland work together to regulate testosterone production through the release of specific hormones. The hypothalamus, located in the brain, produces gonadotropin-releasing hormone (GnRH), which signals the anterior pituitary gland to release LH and follicle-stimulating hormone (FSH). LH directly stimulates the Leydig cells in the testes to produce testosterone, while FSH plays a complementary role in spermatogenesis.
Disruptions in this hormonal cascade can lead to hypogonadism, a condition characterized by insufficient testosterone production. Various factors, including chronic stress, poor nutrition, and certain medical conditions, can impair the function of the hypothalamic-pituitary-gonadal axis, leading to hormonal imbalances. Understanding the central role of these brain structures in testosterone regulation highlights the interconnected nature of endocrine health.
Other Sources of Testosterone Production in the Male Body
While the testes are the primary site of testosterone production, small amounts of testosterone are also synthesized in the adrenal glands. Located atop the kidneys, the adrenal glands produce various steroid hormones, including dehydroepiandrosterone (DHEA), which serves as a precursor to testosterone. Although adrenal testosterone production is significantly lower than testicular synthesis, it can contribute to overall androgen levels, particularly in cases of testicular dysfunction.
The adrenal glands play a crucial role in the body’s hormonal balance, producing a range of different hormone types essential for metabolism, immune function, and stress response. Cortisol, another steroid hormone produced by the adrenal glands, can interact with testosterone levels, as chronic stress and elevated cortisol can suppress testosterone synthesis. Maintaining adrenal health through proper stress management and lifestyle choices can support optimal testosterone production in males.
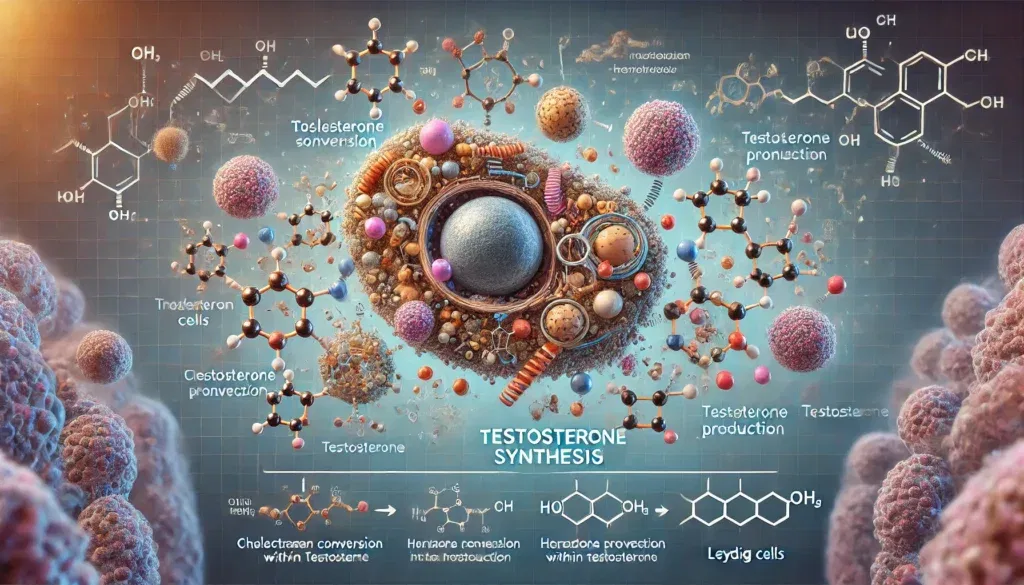
The Conversion of Testosterone in the Male Body
Once produced, testosterone does not remain in a singular form but is metabolized and converted into other biologically active molecules. One of the most well-known conversions is the transformation of testosterone into dihydrotestosterone (DHT) by the enzyme 5-alpha reductase. DHT is a more potent androgen responsible for the development of male secondary sexual characteristics, including facial hair growth, deepening of the voice, and prostate health.
Additionally, testosterone can be aromatized into estrogen, primarily estradiol, through the action of the enzyme aromatase. While estrogen is often associated with female physiology, it is also essential for males, playing a role in bone health, cardiovascular function, and brain activity. An imbalance in testosterone-to-estrogen conversion can lead to conditions such as gynecomastia, where excess estrogen leads to the development of breast tissue in males. Understanding the pathways through which testosterone is converted highlights the hormone’s versatility and impact on various physiological processes.
Factors That Influence Testosterone Production
Numerous factors influence testosterone production in males, ranging from genetic predisposition to lifestyle choices. Nutrition plays a fundamental role, as deficiencies in essential nutrients such as zinc, vitamin D, and healthy fats can impair testosterone synthesis. Regular physical activity, particularly resistance training and high-intensity interval training (HIIT), has been shown to support optimal testosterone levels, while chronic stress and poor sleep quality can suppress production.
Age is another key determinant of testosterone levels. Testosterone production typically peaks in early adulthood and gradually declines with age. This decline, known as andropause or age-related hypogonadism, can lead to symptoms such as decreased energy, loss of muscle mass, and diminished sexual function. While this decline is natural, lifestyle interventions, including proper diet, exercise, and stress management, can help mitigate its effects and promote healthy aging.
The Importance of Maintaining Healthy Testosterone Levels
Testosterone is essential for multiple aspects of male health, and maintaining optimal levels is critical for overall well-being. Low testosterone, or hypogonadism, can lead to a variety of symptoms, including fatigue, depression, erectile dysfunction, and decreased cognitive function. Long-term testosterone deficiency can also contribute to an increased risk of osteoporosis, metabolic disorders, and cardiovascular disease.
There are several approaches to optimizing testosterone levels naturally. Dietary strategies emphasizing protein, healthy fats, and micronutrients essential for hormone production can support testicular function. Strength training and adequate sleep help regulate hormonal balance, while stress management techniques such as meditation and mindfulness can prevent excessive cortisol production, which can suppress testosterone synthesis. For individuals with clinically low testosterone, hormone replacement therapy (HRT) may be an option under the guidance of a healthcare professional.
Frequently Asked Questions (FAQ) on Testosterone Production
1. What gland produces testosterone, and how does it regulate hormone levels?
The primary gland responsible for testosterone production is the testes in males, with a smaller amount produced by the adrenal glands. The hypothalamus and pituitary gland regulate testosterone levels by releasing gonadotropin-releasing hormone (GnRH) and luteinizing hormone (LH), respectively. When testosterone levels drop, the hypothalamus signals the pituitary to release more LH, which stimulates the testes to produce more testosterone. In turn, when testosterone levels rise, this feedback loop reduces LH production, helping to maintain hormonal balance. This regulatory system ensures that testosterone levels stay within an optimal range for bodily functions like muscle growth, bone density, and reproductive health.
2. In what structure is testosterone produced, and how does it affect the body?
Testosterone is primarily produced in the Leydig cells, located within the testes. These cells respond to signals from the pituitary gland, ensuring a steady production of testosterone throughout a man’s life. Once released into the bloodstream, testosterone influences various target organs, including muscles, bones, and the reproductive system. It plays a crucial role in male secondary sexual characteristics such as facial hair growth, voice deepening, and increased muscle mass. Additionally, testosterone has cognitive effects, impacting mood, motivation, and cognitive function.
3. What is testosterone converted to in the male body, and why is this conversion important?
In the male body, testosterone is converted into two key hormones: dihydrotestosterone (DHT) and estrogen. The enzyme 5-alpha reductase converts testosterone into DHT, which is more potent and responsible for male traits such as beard growth and prostate development. Aromatase converts some testosterone into estrogen, which is essential for bone health, mood regulation, and cardiovascular function. The balance between testosterone, DHT, and estrogen is vital for overall health, and imbalances can lead to issues such as hair loss, gynecomastia, or hormonal deficiencies.
4. Where is testosterone found in the body outside of the testes?
Although the testes produce most of the body’s testosterone, small amounts are also synthesized by the adrenal glands, located above the kidneys. These glands produce different hormone types, including androgens, which contribute to overall testosterone levels. In females, the ovaries produce a small amount of testosterone, which is crucial for maintaining libido and muscle strength. Additionally, testosterone is found in various tissues, including fat and muscle, where it plays a role in energy metabolism and muscle maintenance. The body’s ability to convert precursor hormones into testosterone also ensures that levels remain sufficient even under stressful conditions.
5. Which cells produce testosterone, and what factors influence their function?
Leydig cells in the testes are the primary producers of testosterone in males. These cells function optimally when stimulated by luteinizing hormone (LH), which is secreted by the pituitary gland. Several factors influence Leydig cell function, including age, lifestyle, and overall health. For example, obesity, chronic stress, and poor diet can reduce testosterone production, while regular exercise and proper nutrition can enhance it. Maintaining healthy Leydig cell function is essential for preserving testosterone levels and supporting male reproductive and overall well-being.
6. What produces testosterone in males, and can production be naturally boosted?
Testosterone is primarily produced by the testes, but production can be influenced by lifestyle choices and overall health. Adequate sleep, a diet rich in healthy fats, and regular physical activity can help maintain optimal testosterone levels. Strength training and high-intensity interval training (HIIT) have been shown to increase testosterone production naturally. Additionally, reducing stress and avoiding excessive alcohol consumption can prevent the suppression of testosterone synthesis. Certain micronutrients like zinc and vitamin D also play a crucial role in testosterone production.
7. How does the body produce testosterone, and what role do hormones play?
Testosterone production begins in the brain, where the hypothalamus releases gonadotropin-releasing hormone (GnRH). This hormone signals the pituitary gland to produce luteinizing hormone (LH), which then stimulates the Leydig cells in the testes to produce testosterone. The body maintains testosterone levels through a feedback loop that adjusts hormone secretion based on circulating testosterone levels. Other hormones, such as insulin-like growth factor 1 (IGF-1) and cortisol, can also influence testosterone production. Proper endocrine function is essential for sustaining healthy testosterone levels and overall hormonal balance.
8. What gland is responsible for sex hormones, and how do these hormones interact?
The gonads (testes in males and ovaries in females) are the primary glands responsible for sex hormone production. The adrenal glands also contribute by producing small amounts of androgens and estrogens. These hormones regulate various physiological processes, including sexual development, metabolism, and immune function. In males, testosterone is secreted by the testes and converted into DHT and estrogen as needed. The interaction between sex hormones is crucial for maintaining reproductive health, muscle mass, and cognitive function.
9. What gland secretes estrogen, and how does it relate to testosterone?
Estrogen is primarily secreted by the ovaries in females, but in males, small amounts are produced by the testes and adrenal glands. Additionally, testosterone is converted to estrogen in the male body through the enzyme aromatase. While often considered a female hormone, estrogen plays essential roles in men, including supporting bone density and cardiovascular health. Excess estrogen levels in men can lead to unwanted effects such as fat accumulation and decreased libido. Maintaining a proper balance between testosterone and estrogen is crucial for overall health and hormonal equilibrium.
10. Define testosterone in psychology and its impact on behavior.
In psychology, testosterone is often linked to traits such as confidence, competitiveness, and aggression. Studies suggest that higher testosterone levels can influence risk-taking behaviors, motivation, and social dominance. However, testosterone also affects cognitive function, contributing to problem-solving abilities and decision-making. Low testosterone levels have been associated with symptoms of depression, fatigue, and reduced motivation. Understanding the psychological effects of testosterone helps in managing mental health and optimizing performance in various aspects of life.
Conclusion: Understanding and Supporting Testosterone Production
Testosterone is a cornerstone of male health, influencing everything from physical strength and sexual function to cognitive well-being and metabolic balance. Understanding the intricate process of how the body produces testosterone, the key glands and cells involved, and the factors that influence its levels can empower individuals to take proactive steps in maintaining optimal hormonal health. The testes, guided by the hypothalamic-pituitary-gonadal axis, serve as the primary site of testosterone synthesis, while additional contributions from the adrenal glands and metabolic conversions further influence its effects in the body.
By adopting a lifestyle that supports endocrine function, including proper nutrition, regular exercise, and stress management, men can optimize their testosterone levels naturally. Awareness of the potential disruptions to testosterone production, whether from aging, lifestyle choices, or medical conditions, allows for early intervention and informed decision-making. As research continues to uncover the complexities of hormonal regulation, a deeper understanding of testosterone’s role in male physiology will further enhance strategies for maintaining long-term health and vitality.
testosterone production sites, Leydig cells function, hormone regulation in men, endocrine system male health, testosterone metabolism, male hormonal balance, adrenal androgens, testosterone conversion pathways, testosterone health benefits, optimizing testosterone naturally, male endocrine health, HPG axis function, testosterone decline with age, lifestyle impact on testosterone, testosterone deficiency symptoms, testosterone and brain health, resistance training and testosterone, hormone replacement therapy for men, testosterone boosting nutrients, androgen production process
Further Reading:
8 Proven Ways to Increase Testosterone Levels Naturally
Disclaimer: The information provided in this article is for general informational purposes only. The content does not constitute professional advice of any kind, including but not limited to medical, legal, or financial advice. HisHealthMag and its contributors make no representations or warranties regarding the accuracy, completeness, or reliability of the information presented. Always seek the advice of a qualified professional for any specific concerns or questions you may have. Neither HisHealthMag nor its authors assume any responsibility or liability for any actions taken based on the information provided in this article. The views and opinions expressed are those of the author(s) and do not necessarily reflect the official policy or position of HisHealthMag.