Understanding the complex nutritional needs of individuals with stage three kidney failure requires a detailed and nuanced approach. At this stage, the kidneys are moderately impaired and struggling to maintain the body’s internal equilibrium, especially concerning waste product elimination and nutrient balance. A well-formulated meal plan that integrates high-quality protein while respecting renal limitations can significantly influence disease progression, symptom management, and overall well-being. The role of nutrition, particularly a structured stage three kidney failure diet, cannot be overstated in supporting kidney health and prolonging function in the face of chronic kidney disease.
You may also like : The Ultimate Guide to Choosing a High Protein Diet Name That Fits Your Goals
Many people associate kidney disease with the need for a low-protein diet, and while that can be true in later stages, stage three presents a unique opportunity. Moderate protein intake, especially from high-biological-value sources, plays a critical role in preserving muscle mass, maintaining immune function, and providing necessary amino acids for healing and repair. The goal is to strike a delicate balance: avoiding protein overload that burdens the kidneys while ensuring sufficient intake to prevent malnutrition. This article explores the rationale behind a high-protein meal plan tailored to stage three kidney failure, highlights evidence-based dietary strategies, and presents a comprehensive, practical roadmap for those navigating this medical challenge.
Decoding Stage Three Kidney Failure and Nutritional Demands
Stage three kidney failure, often referred to more precisely as stage 3 chronic kidney disease (CKD), signifies a moderate decline in kidney function. With a glomerular filtration rate (GFR) between 30 and 59 mL/min, individuals are likely to experience subtle symptoms like fatigue, fluid retention, and changes in urination patterns. However, it is in this phase that proactive nutritional intervention holds the power to delay further deterioration.
The dietary landscape at this stage is more permissive than in later stages, allowing for strategic nutritional planning that includes controlled yet adequate protein intake. It is a critical point for dietary education, habit reformation, and introducing nutrient-dense foods that support kidney resilience. Key dietary considerations involve monitoring sodium, potassium, phosphorus, and fluid intake, along with careful evaluation of protein quality and quantity. This is where a personalized CKD stage 3 diet plan becomes invaluable, aligning nutrient intake with biochemical parameters and individual needs.

High-Protein Nutrition: Why It Matters in CKD Stage 3
In stage three of kidney failure, protein intake becomes a balancing act between preventing muscle wasting and avoiding excess nitrogen waste that stressed kidneys cannot efficiently excrete. For many individuals, the instinct to reduce protein to protect kidney function may lead to unintended malnutrition, muscle loss, and compromised immune function. Instead, incorporating high-biological-value proteins—those that provide all essential amino acids—in moderate amounts can support tissue repair and energy metabolism.
Emerging research suggests that patients with stage 3 CKD benefit from individualized protein prescriptions. While generalized guidelines often recommend 0.6 to 0.8 grams of protein per kilogram of ideal body weight, this can be cautiously increased to 1.0 to 1.2 grams for those who are physically active, recovering from illness, or at risk of muscle loss. Emphasis should be placed on protein sources that are easier on the kidneys, such as egg whites, lean poultry, tofu, Greek yogurt, and certain plant-based proteins, depending on the individual’s phosphorus and potassium levels.
Creating a high-protein meal plan for a stage three kidney failure diet requires more than just choosing the right proteins. It also demands attention to meal timing, cooking methods that reduce phosphorus and potassium content (like boiling or leaching), and pairing proteins with kidney-safe carbohydrates and vegetables. Ensuring that these meals also support blood sugar control, blood pressure regulation, and electrolyte balance is essential, as many individuals with CKD also have comorbid conditions such as diabetes or hypertension.
The Role of Macronutrients in the Stage Three Kidney Failure Diet
While protein is a focal point of this dietary approach, carbohydrates and fats must not be overlooked. Carbohydrates serve as the primary energy source, helping to spare protein from being used for energy. Complex carbohydrates such as oats, quinoa, barley, and whole grain bread (within potassium limits) are ideal, offering sustained energy and fiber without spiking blood glucose levels. In contrast, simple sugars should be minimized, particularly in those with diabetes, to prevent added strain on kidney function.
Fats are equally important in the stage three kidney failure diet, particularly heart-healthy monounsaturated and polyunsaturated fats. These fats support cardiovascular health, reduce inflammation, and provide calorie density when appetite or food volume is limited. Avocados (if potassium levels permit), olive oil, flaxseeds, and fatty fish like salmon and mackerel are excellent sources. Saturated fats and trans fats, often found in processed meats and baked goods, should be avoided to prevent compounding cardiovascular risks that are elevated in CKD.

Micronutrient Management: Navigating Sodium, Potassium, and Phosphorus
One of the most intricate aspects of managing a diet for chronic kidney disease stage 3 involves regulating electrolyte intake. Excess sodium contributes to fluid retention and hypertension, exacerbating kidney damage. Processed foods, canned goods, and restaurant meals are often saturated with hidden sodium and should be limited. Cooking at home, reading labels, and using fresh herbs and spices as flavor enhancers can substantially reduce sodium intake.
Potassium presents a more nuanced challenge. While essential for muscle and nerve function, elevated potassium levels (hyperkalemia) can be life-threatening for CKD patients. Many fruits and vegetables that are otherwise healthy—like bananas, potatoes, oranges, and spinach—may need to be limited or prepared in ways that reduce their potassium content. Leaching vegetables or choosing lower-potassium alternatives, such as apples, berries, green beans, and cauliflower, can help manage this risk while preserving nutritional quality.
Phosphorus, predominantly found in dairy products, nuts, seeds, legumes, and processed foods with phosphate additives, must also be closely monitored. As kidney function declines, phosphorus can accumulate in the blood, leading to bone and cardiovascular complications. Opting for fresh foods and checking labels for hidden phosphates are essential strategies for adhering to a renal diet. If needed, phosphate binders may be prescribed by a healthcare provider.
Constructing the Ideal High-Protein Day: Sample Meal Plan for Stage 3 CKD
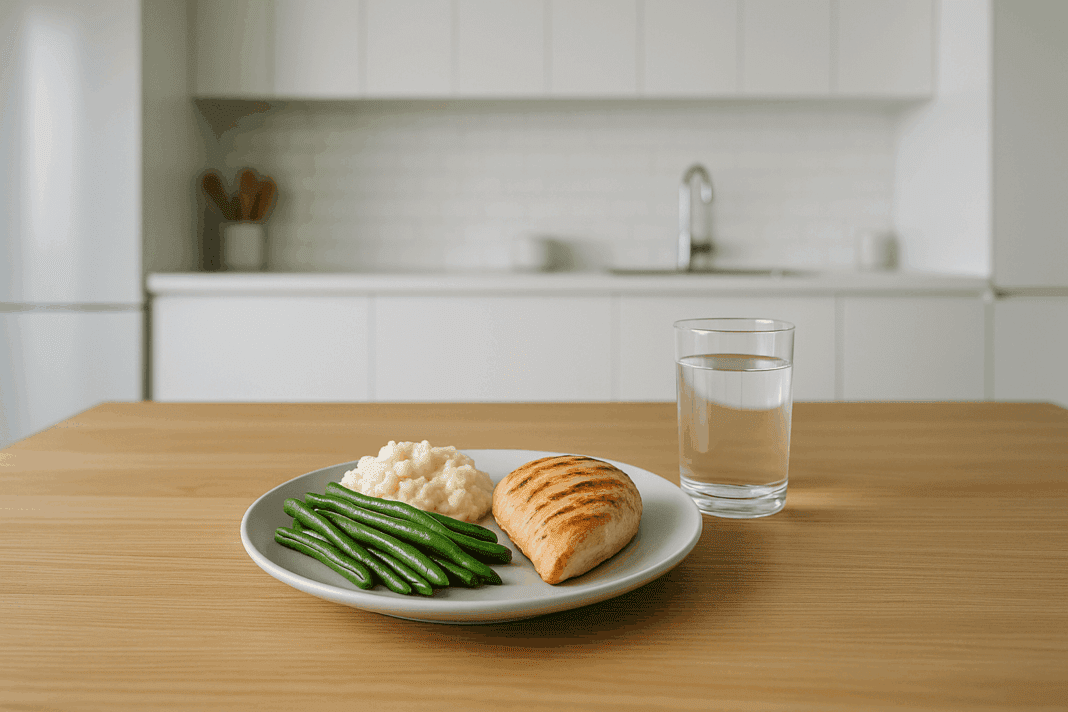
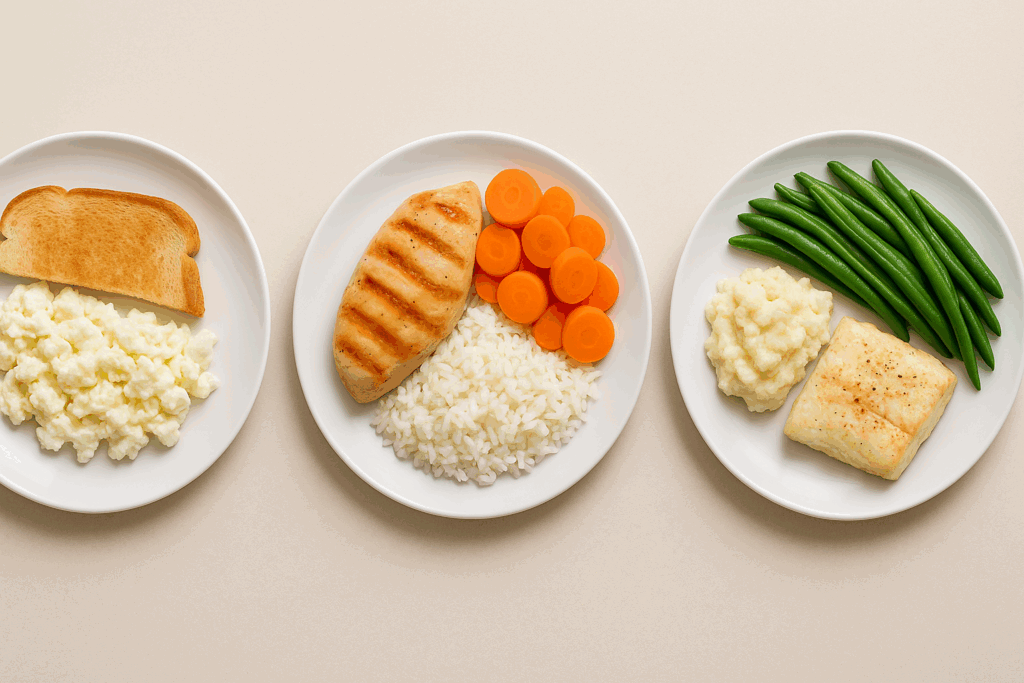
A successful high-protein meal plan for stage three kidney failure must be carefully structured to provide essential nutrients without overburdening the kidneys. A typical day might begin with a protein-rich yet kidney-conscious breakfast, such as scrambled egg whites with bell peppers and a slice of white toast topped with a small amount of unsalted butter. This combination delivers high-quality protein and energy while keeping sodium, phosphorus, and potassium in check.
Lunch could include a grilled chicken breast paired with rice and roasted carrots, offering lean protein, complex carbohydrates, and beta-carotene without overwhelming the kidneys. A mid-afternoon snack of unsalted rice cakes topped with cream cheese or a small serving of Greek yogurt can provide additional protein and calcium without excess phosphorus.
Dinner might feature baked cod seasoned with lemon and herbs, served alongside steamed green beans and mashed cauliflower. This low-potassium, high-protein meal supports renal health while delivering flavor and satiety. Beverages should be carefully chosen; water is best, while phosphorus-laden soft drinks or potassium-rich fruit juices should be minimized. Herbal teas or diluted apple juice may be appropriate depending on individual potassium levels.
Practical Tips for Long-Term Adherence to a Stage Three Kidney Failure Diet
One of the greatest challenges in managing CKD through diet is sustainability. A successful stage three kidney failure diet must not only meet nutritional goals but also be enjoyable, culturally appropriate, and adaptable to lifestyle factors such as work schedules and family dynamics. To support long-term adherence, patients should be encouraged to cook in batches, experiment with low-sodium seasonings, and involve family members in meal planning.
Keeping a food diary can help identify trigger foods, track nutrient intake, and ensure compliance with dietary goals. Working with a renal dietitian is invaluable, as they can tailor meal plans to individual preferences, lab values, and comorbidities. Additionally, understanding food labels, learning how to prepare meals that preserve flavor without harmful additives, and building a repertoire of go-to meals can help transform dietary restrictions into an empowering routine.
Stage Three Kidney Failure Diet: Managing Protein Intake with Confidence
A critical insight for patients and caregivers is recognizing that protein restriction is not a one-size-fits-all mandate. In the context of a stage three kidney failure diet, the emphasis should be on individualized, high-quality protein consumption rather than arbitrary limitations. This approach allows for improved patient outcomes, higher quality of life, and potentially slower disease progression.
Educating patients on protein portion sizes, cooking methods that reduce phosphate content (such as boiling), and the importance of spreading protein intake evenly throughout the day is essential. Additionally, understanding that plant-based proteins may require pairing with other foods to form complete proteins can help expand dietary options without sacrificing nutritional adequacy.
Monitoring lab values like serum creatinine, urea nitrogen, and estimated GFR can guide adjustments in protein intake over time. Rather than rigidly adhering to outdated low-protein models, patients should embrace a dynamic, responsive diet plan rooted in evidence, personalized care, and an understanding of how dietary choices affect kidney workload and systemic health.
Addressing Common Misconceptions About CKD Diets
Many misconceptions persist about what constitutes a proper chronic kidney disease diet, often leading to confusion or unnecessary dietary restrictions. One common myth is that all protein is harmful in CKD. While excessive protein can accelerate kidney decline, moderate amounts of high-quality protein are essential for maintaining strength, immunity, and metabolic function.
Another widespread error is believing that all fruits and vegetables must be eliminated due to potassium content. In reality, many low-potassium fruits and vegetables are safe and beneficial, offering essential vitamins, fiber, and antioxidants. Overly restrictive diets not only lower quality of life but also increase the risk of nutritional deficiencies.
Similarly, it is not true that all fats are harmful in a renal failure diet. Healthy fats can support heart health, reduce inflammation, and serve as vital energy sources, especially in individuals with decreased appetite. Clarifying these myths with factual, evidence-based information can empower patients and reduce anxiety surrounding food choices.

Balancing the Emotional and Psychological Aspects of a Renal Diet
Living with chronic kidney disease involves more than physiological adjustments; the emotional and psychological aspects of following a renal impairment diet must also be acknowledged. Dietary restrictions can feel overwhelming, especially when they intersect with social activities, cultural traditions, or long-standing food habits. Feelings of loss, anxiety, or isolation are not uncommon.
Support groups, counseling, and open communication with healthcare providers can help mitigate these emotional burdens. Incorporating favorite flavors in new, kidney-friendly ways, sharing meals with family, and celebrating dietary victories—no matter how small—can all contribute to a positive mindset. Remember, the goal is not perfection but progress. Encouragement, compassion, and shared responsibility go a long way in sustaining dietary changes.
Emphasizing Plant-Based Protein Without Sacrificing Nutritional Adequacy
The adoption of plant-based diets in CKD has sparked much debate due to concerns over phosphorus and potassium content. However, when carefully constructed, a plant-based chronic kidney failure diet can meet protein needs while reducing the acid load and oxidative stress associated with animal proteins.
Soy products, seitan, quinoa, and tofu provide complete proteins and may be suitable for many stage 3 CKD patients when portion-controlled. Phosphorus from plant sources is less bioavailable than from animal sources, meaning it is absorbed less efficiently by the body. Soaking and cooking legumes, avoiding phosphate additives, and pairing plant proteins with low-potassium vegetables further enhances safety.
Moreover, plant-based diets have been shown to lower blood pressure, improve lipid profiles, and reduce inflammation, all of which are desirable outcomes in CKD management. These benefits align with the broader goals of a diet for chronic kidney disease stage 3.

Hydration Strategies and the Role of Water Quality
Although fluid overload is a concern in later stages of CKD, in stage 3, maintaining optimal hydration supports kidney filtration and blood pressure regulation. Water intake must be individualized based on urine output, comorbidities like heart failure, and sodium status. Emphasis should be placed on consistent, moderate fluid consumption throughout the day rather than excessive intake in one sitting.
Emerging research suggests that water quality may also influence kidney outcomes. Contaminants such as heavy metals, fluoride, or high sodium content in tap water may exert additional renal stress over time. Considering filtered water or testing local water supplies can offer peace of mind and potentially reduce toxic exposure in those with compromised kidney function.
Gut Microbiome and Its Influence on Kidney Health
Recent studies have uncovered a complex relationship between the gut microbiome and kidney function. Dysbiosis, or an imbalance in gut bacteria, can contribute to increased production of uremic toxins like indoxyl sulfate and p-cresyl sulfate, which further strain kidney function.
Incorporating prebiotic and probiotic foods into the stage 3 kidney diet plan may support a healthier gut flora. Prebiotics such as inulin (found in asparagus, onions, and leeks) and probiotics from yogurt or fermented vegetables (low in sodium and potassium) can help reduce the generation of these nephrotoxic substances. Supplements like bifidobacteria or lactobacillus strains, when deemed appropriate, can serve as adjunct therapies under medical supervision.
Further, resistant starches, found in cooled potatoes and certain legumes, can improve glycemic control and reduce inflammation, offering multifaceted benefits in CKD management. By supporting the gut-kidney axis, patients may experience reduced toxin load and slower disease progression.
Personalized Nutrition Based on Genetic and Metabolic Markers
One of the most promising developments in dietary management of stage 3 CKD is the use of personalized nutrition plans based on genetic and metabolic biomarkers. These approaches utilize data such as genetic polymorphisms affecting phosphorus metabolism, insulin sensitivity, or inflammatory pathways. Nutrigenomic testing can provide insights into how a patient metabolizes nutrients, allowing healthcare providers to fine-tune a kidney diet that meets the individual’s unique biochemical profile.
For example, patients with certain variants in the FGF23 or Klotho genes may be more susceptible to phosphate retention and may benefit from more aggressive phosphorus limitation, even in early CKD. Others may have higher inflammatory markers that respond favorably to a Mediterranean-style renal diet enriched with anti-inflammatory compounds. While still in its early stages, this personalized approach moves beyond a one-size-fits-all renal failure diet and paves the way for precision medicine.
Advanced Glycation End Products (AGEs) and CKD Progression
Advanced glycation end products (AGEs) are harmful compounds formed when proteins or fats combine with sugars in the bloodstream. They are also found in high amounts in grilled, fried, and processed foods. AGEs contribute to oxidative stress and inflammation, accelerating the decline in kidney function.
Reducing dietary AGE intake is a novel yet evidence-backed intervention for patients following a stage three kidney failure diet. Cooking methods such as steaming, boiling, or poaching are preferred over frying or roasting. Foods that are naturally lower in AGEs, such as fresh fruits, vegetables, and whole grains, offer protection and are often compatible with renal dietary restrictions when carefully selected for potassium and phosphorus content. Including antioxidant-rich foods like red cabbage, blueberries, or green tea can also counter the damaging effects of AGEs, offering a holistic complement to traditional kidney diets.
Physical Activity and Its Synergy with Nutritional Strategies
Although the focus is often on diet alone, the integration of physical activity into CKD care should not be underestimated. Regular, moderate exercise enhances insulin sensitivity, supports muscle mass retention, and improves cardiovascular function—all of which reduce the systemic burden on the kidneys.
Low-impact activities such as walking, swimming, or yoga are particularly well-suited for those with stage 3 CKD. Importantly, maintaining muscle mass allows for better nitrogen metabolism, meaning that the body utilizes protein more efficiently. This synergy between exercise and a high-protein stage three kidney failure diet supports strength and functional independence.
The Role of Supplementation and Functional Foods in a CKD Diet Plan
In some cases, even the most carefully constructed diet for CKD stage 3 may fall short in certain nutrients due to the need to restrict specific foods. This is where supplementation, guided by a healthcare provider or renal dietitian, may play a role. Commonly needed supplements may include vitamin D, iron, B-complex vitamins, or omega-3 fatty acids.
Functional foods—those with health-promoting properties beyond basic nutrition—can also enhance a chronic kidney failure diet. For example, pomegranate juice (in limited, potassium-monitored amounts) has antioxidant properties that may protect against inflammation and oxidative stress. Similarly, turmeric, flaxseed, and ginger have shown promise in supporting renal health, though their use should be tailored to individual lab values and overall dietary balance.
Cultural and Social Considerations in Dietary Planning
One often overlooked but vital aspect of dietary compliance is the cultural and social context of food. Meals are more than just fuel; they are expressions of identity, tradition, and community. Ignoring these dimensions can lead to non-adherence and emotional distress.
Adapting a renal disease diet to include culturally relevant dishes, such as modifying spice blends, using traditional cooking methods, or substituting ingredients, can enhance engagement. Encouraging communal meal preparation and involving family members in the dietary journey fosters shared responsibility and emotional support.
Frequently Asked Questions: Optimizing Your Stage Three Kidney Failure Diet for Better Outcomes
1. What are some often-overlooked lifestyle changes that can support a stage three kidney failure diet?
While most people focus on limiting sodium and protein intake in a stage three kidney failure diet, incorporating behavioral and environmental shifts can significantly improve outcomes. For instance, maintaining a consistent meal schedule can help stabilize blood glucose and phosphorus levels, both critical for slowing CKD progression. Avoiding late-night snacking helps reduce the workload on the kidneys during their natural nighttime filtration cycle. It’s also valuable to adopt stress-reducing habits such as meditation or nature walks, which have been shown to reduce systemic inflammation—a contributor to kidney damage. When paired with a well-structured ckd diet plan, these practices enhance the effectiveness of nutrient management and improve long-term renal resilience.
2. How can social eating habits complicate adherence to a chronic kidney disease diet?
Social gatherings often include foods high in sodium, phosphorus, and protein—ingredients that are restricted in a chronic kidney disease diet. Dining out can be especially challenging, as restaurant meals are not typically tailored for a kidney disease renal diet. Even well-meaning friends may not understand the need for specific dietary limits. One effective strategy is to call ahead and request ingredient lists or bring a renal-safe dish to share. Being transparent about your dietary needs not only educates others but also creates a supportive environment that reinforces your renal impairment diet goals.
3. What unexpected foods may be harmful for those following a ckd stage 3 diet?
Many assume that “healthy” foods are always safe for kidney health, but this isn’t the case for a ckd stage 3 diet. Foods like bran cereal, brown rice, and bananas—often lauded for their nutrient content—can contain excessive phosphorus or potassium. Similarly, dairy alternatives such as almond milk may include phosphate additives that burden already-impaired kidneys. Even some plant-based protein powders contain hidden sodium and potassium that can disrupt your kidney insufficiency diet. Reading labels for “phos” additives and opting for fresh, whole, and minimally processed foods is essential for managing a renal disease diet effectively.
4. What role does hydration play in a diet for chronic kidney disease stage 3?
Hydration is critical, but it must be carefully balanced in a diet for chronic kidney disease stage 3. While adequate fluid intake helps flush toxins and prevent kidney stones, excessive fluid can lead to complications such as fluid retention, hypertension, and edema—especially when kidney function is diminished. In CKD stage 3, fluid recommendations vary based on blood pressure, sodium intake, and urine output. It’s best to sip fluids throughout the day rather than drink large amounts at once. Tracking fluid intake as part of a comprehensive kidney failure diet plan allows for fine-tuning hydration without overloading the renal system.
5. How can psychological health impact the effectiveness of a renal insufficiency diet?
Chronic illness often triggers stress, anxiety, and depression, which can negatively affect compliance with a renal insufficiency diet. Emotional distress may lead to poor dietary choices, binge eating, or skipping meals altogether. Cognitive behavioral therapy (CBT) and mindfulness practices have shown promise in improving dietary adherence in CKD patients. In fact, structured mental health support programs have been linked with improved biochemical markers and reduced disease progression. By addressing the emotional component of living with CKD, patients are more likely to maintain their renal failure diet and experience better long-term outcomes.
6. Is it possible to tailor a stage three kidney failure diet for other coexisting conditions like diabetes or heart disease?
Yes, and in fact, it’s essential. Many patients following a stage three kidney failure diet also manage diabetes or cardiovascular issues. In such cases, a dual-focus meal plan can be customized to control blood glucose while still adhering to renal diet limits. For example, using low-glycemic vegetables like cauliflower instead of starchy ones like potatoes can stabilize blood sugar and reduce potassium intake. Lean proteins like egg whites can support both a heart-healthy and a kidney disease renal diet. Coordination between a registered dietitian and nephrologist ensures that your ckd disease diet complements all your health concerns without nutritional gaps.
7. What nutrient do you increase in CKD and why is it critical at stage 3?
A frequently asked but complex question is: what nutrient do you increase in CKD, particularly during stage 3? The answer depends on the individual’s lab results, but in many cases, dietary fiber is emphasized. Fiber helps reduce systemic inflammation and supports gut microbiota, which indirectly reduces uremic toxins that the kidneys would otherwise filter. Soluble fiber can also assist in stabilizing blood sugar and cholesterol—both crucial for slowing kidney disease progression. While other nutrients like iron or vitamin D may be supplemented depending on lab values, fiber-rich foods that fit within renal diet limits—like peeled apples and white beans—offer multidimensional benefits in a kidney insufficiency diet.
8. How can a plant-based approach enhance the benefits of a kidney damage diet?
Plant-based diets are increasingly recommended as a cornerstone of a kidney damage diet because they reduce the burden of metabolic byproducts like urea and acid. Unlike animal proteins, plant proteins yield fewer waste compounds and lower phosphorus levels, supporting a safer ckd diet plan. Additionally, the high antioxidant content in plant foods can reduce oxidative stress—a contributor to renal decline. However, not all plant foods are safe; high-potassium choices like spinach and avocados must be moderated. A renal impairment diet rooted in plant-based principles but curated for phosphorus and potassium can significantly support kidney function and delay dialysis.
9. How does cultural cuisine fit into a diet for kidney disease without compromising flavor?
Adapting cultural foods into a diet for kidney disease is entirely possible with thoughtful substitutions. For example, in Asian cuisine, using low-sodium soy sauce or coconut aminos instead of traditional soy can protect against sodium overload. In Mediterranean diets, substituting canned olives with fresh herbs maintains flavor without excess sodium or phosphorus. Cooking methods like steaming and grilling allow for flavor retention without added fat or salt—key for a kidney disease renal diet. Learning how to reinterpret traditional dishes through a renal failure diet lens helps patients preserve cultural identity while staying within renal diet limits.
10. What future innovations could improve the personalization of a stage 3 kidney diet?
Emerging technologies in nutrigenomics and microbiome mapping hold promise for customizing a stage 3 kidney diet. DNA-based dietary recommendations may soon offer insights into how individuals metabolize sodium, phosphorus, and other renal stressors. Wearable health devices could monitor hydration, potassium levels, and blood pressure in real time, allowing for immediate adjustments in your ckd stage 3 diet. Moreover, AI-driven meal planning tools are already being piloted to support diet for chronic kidney disease stage 3 with tailored recipes and grocery lists. These innovations will not only simplify adherence but also enhance outcomes in those managing a chronic kidney failure diet.
Conclusion: Building a Sustainable and Empowering Stage Three Kidney Failure Diet
The journey of living with stage 3 CKD is one of proactive empowerment, and a thoughtfully crafted stage three kidney failure diet is among the most powerful tools patients have at their disposal. By understanding the body’s evolving nutritional needs and embracing a high-protein meal plan designed to support strength, resilience, and renal function, individuals can take meaningful steps toward managing their condition.
A successful CKD diet plan is not just about restrictions but about rediscovering food through a new lens—where creativity, knowledge, and support intersect. From choosing the right protein sources and managing electrolyte intake to addressing the emotional complexities of dietary change, this journey is one of ongoing learning and adaptation. As science continues to shed light on the nuances of kidney nutrition, the hope is that more individuals with CKD will feel empowered, not limited, by their diets.
By integrating high-protein nutrition into a kidney-conscious lifestyle, patients with stage 3 CKD can preserve muscle mass, enhance quality of life, and potentially delay progression to more advanced disease stages. With the guidance of healthcare professionals and a commitment to self-care, the renal disease diet becomes not a burden but a cornerstone of better health and hopeful living.
Further Reading:
8 Diet and Nutrition Goals for People with Stage 3 Chronic Kidney Disease